Clinical examination includes an abdominal and pelvic (with speculum) examination. The most important ancillary testing are beta hCG levels and a pelvic ultrasound. Other important investigations include blood group, thyroid-stimulating hormone (TSH), and a urine dip. The ultrasound may be able to determine if the pregnancy is intrauterine or extrauterine (ectopic) and if it is viable (fetal cardiac activity) in the case of an intrauterine pregnancy.1 It may also be able to identify more rare causes of bleeding including gestational trophoblastic disease (GTD) or loss of one fetus in a multiple gestation.1
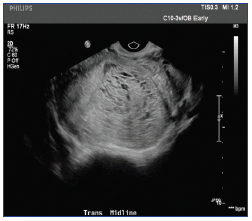
The ultrasound findings in this clinical context suggest a partial molar pregnancy. Molar pregnancy is a tumor of gestational tissue that results from an error in fertilization – either an anuclear ovum is fertilized by a normal spermatozoa or two spermatozoa fertilize a normal ovum.3, 4 Molar pregnancies are either complete or partial, differentiated based on chromosomal patterns and gross morphology, histopathology, and karyotype. 1, 3 Complete molar pregnancies are usually diploid or associated with higher risks, while partial molar pregnancies are usually triploid and about twice as common.2 They are under the classification of GTD and are considered premalignant as they can become malignant, invade the uterus, and less commonly, metastasize.2
The average gestational age of diagnosis is 11.8 weeks and is usually found on ultrasound before symptoms present. It most commonly presents with vaginal bleeding (84% of patients) or pelvic pressure or pain and may have excessive uterine size (28%) or hyperemesis (8%).3 Other less common presentations include anemia, preeclampsia, and hyperthyroidism.3
Rho(D) immunoglobulin after the D&C.3 For women who do not wish to preserve fertility, and usually those older than age 40 years, hysterectomy may be chosen. Pathological assessment of evacuated gestational tissue is important for confirmation of the diagnosis, for follow-up, and determining prognosis.
Prophylactic chemotherapy (usually methotrexate) may reduce the risk of gestational trophoblastic neoplasia (GTN) in cases of complete molar pregnancy and may be considered in cases where followup is a concern or in high-risk patients. It is important to continue to follow beta hCG levels, beginning 48 hours after surgery, to monitor for GTN in all patients. Beta hCG should be checked every 1-2 weeks until less than 5 mU/ml and then can be 1-2 months for the next 6-12 months.2, 3 If these levels increase or remain elevated for several weeks after a complete or partial molar pregnancy, the patient is considered to have GTN.2, 3
The most serious complication of molar pregnancy is GTN. Patients with beta hCG > 175 000 mIU/mL before D&C are at ultra high risk for GTN with a risk of 85% of developing GTN. Out of 82 women, over half developed GTN with D&C alone; however, none of the women who had hysterectomy alone developed GTN. Other potential complications are hyperthyroidism, ovarian theca lutein cysts, preeclampsia, and cardiopulmonary symptoms.8 With evacuation of the mole, all thyroid abnormalities and preeclampsia resolve and cysts will usually regress in the following months as beta hCG levels drop. Cardiopulmonary symptoms include tachypnea, tachycardia, dyspnea, and chest pain, and may show bilateral pulmonary infiltrates on chest x-ray or rales on auscultation. This usually affects women in the second trimester and tends to disappear within hours of D&C.
References
Benson CB, Genest DR, Bernstein MR, et al. Sonographic appearance of first trimester complete hydatidiform moles. Ultrasound Obstet Gynecol 2000; 16:188.
Berkowitz RS, Goldstein DP. Clinical practice. Molar pregnancy. N Engl J Med 2009; 360(16):1639-45.
Berkowitz RS, Goldstein DP, DuBeshter B, et al. Management of complete molar pregnancy. J Reprod Med 1987; 32:634.
Soper JT, Mutch DG, Schink JC. American College of Obstetricians and Gynecologists (ACOG) Practice Bulletin No. 53. Diagnosis and Treatment of Gestational Trophoblastic Disease. Gynecol Oncol 2004; 93(3):575-85.
Soto-Wright V, Bernstein M, Goldstein DP, et al. The changing clinical presentation of complete molar pregnancy. Obstet Gynecol 1995; 86:775.